Deng Hongkui’s team from Peking University published a report in Nature on the research results of using small chemical molecules to induce human Somatic cells to transform into pluripotent stem cells
On April 13, 2022, Deng Hongkui's research team from the School of Life Sciences of Peking University and the Peking University Tsinghua Life United Center published a research paper entitled "Chemical reprogramming of human somatic cells to pluripotent stem cells" online in the international academic journal Nature. It was the first international report on the breakthrough research achievement of using small chemical molecules to induce human Somatic cells to transform into pluripotent stem cells. The use of chemical small molecules to reprogram cell fate (chemical reprogramming) is a new generation of human pluripotent stem cell preparation technology independently developed by China following the "nuclear transfer" and "transcription factor induction", which has solved the "bottleneck" problem of bottom technology for the development of stem cells and Regenerative medicine in China.
Pluripotent stem cells have the characteristics of infinite proliferation and the ability to differentiate into all functional cell types of organisms. These magical characteristics make them have extensive application value in cell therapy, drug screening, disease models, and other fields, and they are the most critical "seed cells" in the field of Regenerative medicine. In the natural development of mammals, pluripotent stem cells only exist briefly in the early stage of embryonic development, and then they will differentiate into various types of Somatic cells that constitute the organism, losing their "seed cell" characteristics. How to reverse this natural development process and make highly differentiated Somatic cell cells regain the multipotential state similar to early embryonic development has always been one of the most important scientific issues in the field of stem cells and Regenerative medicine.
In the 1960s, British scientist John Gurdon developed the nuclear transfer technology in Xenopus laevis. In 1997, Ian Wilmut's team used this technology to prepare cloned sheep Dolly, which proved that highly differentiated Somatic cells of mammals can also be reversed to the initial state of early embryos, and gained the ability to develop into an entire animal individual. In 2006, Shinya Yamanaka, a Japanese scientist, reported that mouse Somatic cell cells can be reprogrammed into pluripotent stem cells (iPS cells) using transgenic methods, which are called induced pluripotent stem cells (iPS cells). The methods of nuclear transfer and introduction of foreign genes have proved that mammalian Somatic cell cells can be reprogrammed to revert to the early stage of embryonic development and regain "pluripotency". These two technologies won the Nobel Prize in Physiology or Medicine in 2012. The establishment of iPS technology has broken the ethical limitations of traditional embryonic stem cells and provided a new method for constructing patient-specific stem cell lines, greatly accelerating the process of clinical application of stem cells. In recent years, clinical trials of cell therapy for Parkinson's disease, diabetes, cancer, and other key diseases have been carried out. However, the current technology system for cell therapy has been developed abroad. Can China have original underlying technologies?
For a long time, Deng Hongkui's team has been committed to developing new methods for regulating cell fate and establishing the underlying technology for preparing stem cells. In 2013, Deng Hongkui's team published an original research achievement in Science magazine, that is, without relying on endogenous substances such as oocytes and transcription factors, only using exogenous chemical small molecules can reverse cell fate, and reprogram mouse Somatic cell cells into chemically induced pluripotent stem cells (CiPS cells). Compared to traditional methods, chemical small molecules are easy to operate and flexible, with strong spatiotemporal regulation and reversible effects, allowing for precise manipulation of cell reprogramming processes. In addition, the small molecule-induced Somatic cell reprogramming technology, as an Unconformity method, avoids the safety problems caused by traditional transgenic operations and is expected to become a safer clinical treatment method. Later, Deng Hongkui's team published articles in Cell, Cell Stem Cell, and other magazines in succession, elaborating on the unique molecular mechanism of chemical reprogramming, and further optimizing the mouse chemical reprogramming system. Subsequently, several research groups, including Xie Xin, Yao Hongjie, Duanqing Pei, Liu Lin, and Zhu Saiyong, repeated and optimized the mouse chemical reprogramming technology using the same or similar chemical small molecule combinations. The research of chemical reprogramming inducing pluripotent stem cells has opened up a new way of Somatic cell reprogramming, which not only helps to better understand the mechanism of cell fate determination and transformation but also brings new possibilities for Regenerative medicine to treat major diseases in the future.
In this study, Deng Hongkui's team reported for the first time the use of chemical reprogramming, which successfully achieved the use of small chemical molecules to induce human Somatic cells into pluripotent stem cells (human CiPS cells). The establishment of this technology has opened up a new path for the preparation of human pluripotent stem cells, making it a crucial step toward clinical application.

Figure 1. New generation induced pluripotent stem cell technology
As an advanced animal, the complexity of human Somatic cell-cell characteristics and steady-state regulation is far from that of mouse Somatic cells. There are many obstacles at the epigenetic level, which severely limit the possibility of stimulating cell plasticity in human Somatic cells. Since 2013, although many international teams have made a lot of attempts inspired by mouse chemical reprogramming, they have failed to solve the chemical reprogramming problem of human Somatic cell cells. This makes it widely recognized in the field that the epigenetic restrictions of human Somatic cells are extremely strict, and it is likely that human Somatic cells cannot be stimulated to acquire pluripotency through chemical reprogramming. Deng Hongkui's team has broken through this bottleneck through long-term persistence and unremitting efforts. The Committed step of this breakthrough was inspired by the regeneration process of lower animals. The Somatic cell cells of lower animals such as newts will spontaneously change their characteristics after being damaged by the outside world, and then obtain certain plasticity through differentiation. With the help of this plastic intermediate state, limb regeneration can be achieved. Along this line of thought, the research team carried out a large number of screenings and a combination of small chemical molecules and finally found that highly differentiated human Somatic cell cells can also undergo similar dedifferentiation under the action of a specific combination of small chemical molecules, obtaining a certain plastic intermediate state. On this basis, the research team ultimately achieved successful induction of human CiPS cells.
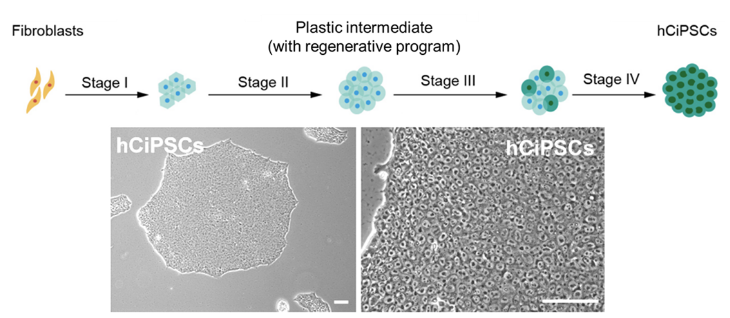
Figure 2. Human CiPS cells induced by chemical reprogramming of human cells
Compared with traditional technology systems, CiPS cell induction technology has irreplaceable advantages such as being safer and simpler, easier to standardize, and easier to regulate. It breaks through the limitations faced by iPS technology and has broad clinical application prospects. 1) In terms of safety, it has been previously demonstrated in mouse CiPS cells that they carry significantly fewer genetic mutations than traditional iPS cells, and the chimeric mice produced do not produce tumors and all live healthy during a 6-month observation period. Meanwhile, pancreatic islet cells derived from human CiPS cell differentiation were transplanted into mice and nonhuman primate models, and no tumor formation was found after long-term observation; 2) In terms of individualized preparation, the research team has now achieved stable induction of human CiPS cells in Somatic cell types from individuals of different ages; 3) In terms of standardized cell preparation, chemical small molecules have a series of characteristics such as simple operation, strong spatiotemporal regulation, reversible action, convenient synthesis and storage, and easy standardized production, making human CiPS cells have irreplaceable advantages in standardized and large-scale production. It should be noted that human CiPS cells can efficiently prepare islet cells, and can safely and effectively improve the blood sugar control of diabetes monkeys, highlighting the great advantages of human CiPS cells as "seed cells" in the safety and effectiveness of treating major diseases. The main results of this study were published in the medical journal Nature Medicine in February this year.
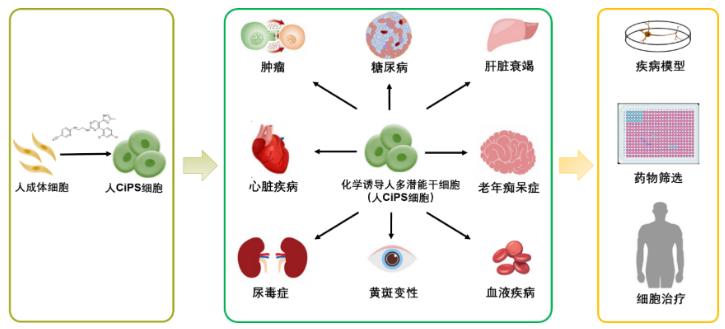
Figure 3. Human CiPS technology has broad potential application prospects in the biomedical field
On this basis, the research team also described the molecular pathway of chemical reprogramming inducing human CiPS cells, revealing the different molecular mechanisms and unique regulatory mechanisms between chemical reprogramming and traditional transcription factor reprogramming. Research has found that the induction of human CiPS occurs in a phased and precise manner, resulting in a special intermediate state in the early stages. Through a detailed comparison of cell properties during the process of regeneration and dedifferentiation with lower animals, the research team confirmed that the early stage of human CiPS cell induction activated gene expression features similar to those of lower animals in the early stage of limb regeneration. More importantly, the research team also found the key signaling pathway regulating this kind of regenerative state, proving that inhibiting excessive inflammatory reactions is crucial for chemical reprogramming to induce human cells to regain the regenerative-like intermediate state. This regeneration intermediate state provides a new idea for studying the reactivation of regeneration genes in human cells and suggests that it is possible to reactivate the plasticity and regeneration potential of human cells only through chemical small molecule combinations in the future, which is expected to promote the application of chemical reprogramming in the direction of tissue and organ regeneration and provide a new possible way for the research of Regenerative medicine.

Figure 4. Molecular mechanism of chemical reprogramming activation and regeneration-related networks
In recent years, Deng Hongkui's team has extended the strategy of chemical reprogramming to different applications of regulating cell fate. The team realized the transformation between different types of Somatic cell cells by using small chemical molecules, and directly reprogrammed skin cells into functional neurons (Cell Stem Cell, 2015; Cell Stem Cell, 2017); Established EPS cells with pluripotent functional characteristics (Cell, 2017); It solved the problem that liver cell function is difficult to maintain in vitro for a long time (Science, 2019), constructed a new Organoid like model with regenerative ability (Cell Research, 2021), and realized in vivo chemical reprogramming (Cell Discovery, 2021). This series of works reflects the universality of chemical small molecules in regulating cell fate.
In summary, the establishment of a chemical reprogramming technology system not only has great significance and value in the clinical application field of pluripotent stem cells but also provides a new perspective and platform for theoretical research on cell fate regulation and regenerative biology. Chemical reprogramming can precisely regulate the fate of cells and is expected to become a General-purpose technology for the efficient preparation of various functional cell types, opening up a new way to treat major diseases.
Deng Hongkui led the study. Deng Hongkui, Dr. Wang Jinlin of Peking University, and Professor Lu Shichun of 301 Hospital are the co-corresponding authors of this research achievement. Guan Jingyang, Wang Guan, Wang Jinlin, Zhang Zhengyuan, Fu Yao, Cheng Lin, Meng Gaofan, and Lv Yulin from Peking University are the main authors of this research achievement. Professor Li Cheng from Peking University provided important guidance for the bioinformatics analysis of this study. This work has been supported by the Peking University Tsinghua Life Sciences United Center, the National Key R&D Program, and the National Natural Science Foundation of China.